Tips For Better Distant Learning Education

Distant Learning
The coronavirus or COVID 19 pandemic has led to widespread challenges. One such challenge is school closures and distant learning nationally. With the implementation of distant learning, families are struggling to instruct their students. Consequently, students are at risk for regression. Students with disability are even more vulnerable to regression since they rely on individualized education plans (IEPs) to learn.
McKinsey & Company (2020) confirmed in recent research that most students are falling behind with distant learning. Here are some tips to promote better distant learning education during the COVID 19 pandemic.
Model Normal, In-Person School Procedures
Daily routine is important when raising children. It teaches them balance and consistency. It also promotes healthy habits. Thus, it is especially important to maintain a daily learning schedule. For instance, settling on a time that learning begins. For most distant learners, school begins at regularly scheduled time like in the classroom setting. Dress your schooler for school; that does not include pajamas. Also, make sure your schooler eats breakfast before screen time.
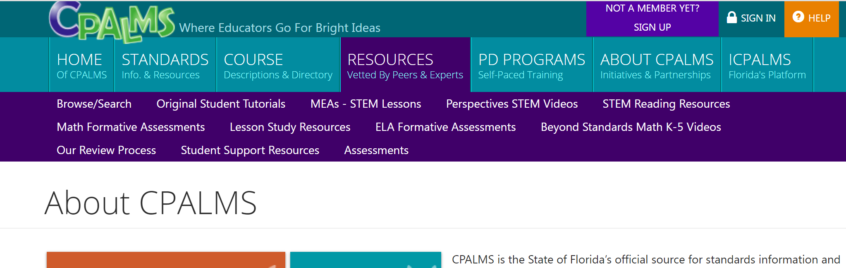
Free State Resources
Many states provide free online resources to educators, parents, and caregiver. For example, the Florida’s CPALMS platform. CPALMS offers free online resources, and interactive tools that help educators effectively implement teaching standards. It is the State of Florida’s official source for standards information and course descriptions. Information and resources are also available to caregivers.
CPALMS is not currently available to non-Florida educators or caregivers. However, interested non-Florida educator and caregivers are encouraged to sign up for notification. Once the new version that will allow all districts, schools, teachers, and parents/caregivers anywhere to subscribe, those interested will be notified. In addition, Access Points supports students with exceptional needs.
Home School Curriculum
You may think that home school curriculum is for the fulltime home schooler. But did you know that you can use homeschool curriculum to supplement your child’s distant learning education? Many online homeschool curriculums offer self-pace, full, and interactive programs to fit your family’s need.
I have tried ABC mouse, Time for Learning, and IXL home school curriculums. IXL is by far my favorite and the only one I currently use. By the way, I am not being paid by IXL. I honestly love the program. They offer comprehensive curriculum, real time diagnostic, personalized guidance, and real time insights. IXL’s language art program has truly helped with language development in my once deemed, non-verbal son.
For those who cannot afford paid home school curriculum, there are other free resources available
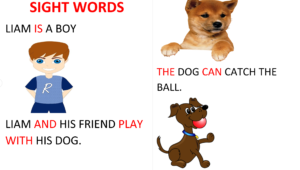
Create Books with Sight Words
Language development is a major priority in our household. Why? Because my son’s major challenge, due to autism spectrum disorder, is receptive and expressive language. A trick I employ to help him read is to create story books with sight words. These story books are created with familiar items around the house to facilitate word- object pairing and functional language. It also improved his understanding of language. Creating a storybook with sight words is fun and simple. It is also one you can do with your schooler.
Use word document or whatever program of your choice. Create a simple and relatable story using sight words. Be sure to highlight sight words and insert colorful images to create a fun story. You can involve your child in the story making process.
Building Common Core Vocabulary
Free gift for Subscribers! Subscribe for your free copy of Building Common Core Vocabulary in Non-verbal Students.











 Though
Though 













 Fast forward about 6.5 years later. I decided to surprise Liam (my son) on his 7th birthday to an evening of horseback riding. Since he had only been around horses once, an event I was sure he didn’t remember, I carefully approached the situation. Still, I had high hopes that he would enjoy the experience. Even though I hoped for a fun experience , the real reason behind the visit was to broaden his experience of different live animals. You see, he has challenges with receptive and expressive language, so, modeling the word with a clear picture was effective in improving his language skills. This technique we took from extensive
Fast forward about 6.5 years later. I decided to surprise Liam (my son) on his 7th birthday to an evening of horseback riding. Since he had only been around horses once, an event I was sure he didn’t remember, I carefully approached the situation. Still, I had high hopes that he would enjoy the experience. Even though I hoped for a fun experience , the real reason behind the visit was to broaden his experience of different live animals. You see, he has challenges with receptive and expressive language, so, modeling the word with a clear picture was effective in improving his language skills. This technique we took from extensive Our Horseback Riding Story
Our Horseback Riding Story So what is therapeutic horseback riding and how does it improve autism associated symptoms? Therapeutic horseback riding (TR) or equine assisted therapy is an activity used with individuals with autism and other special needs. It is used for the purpose of improving physical, emotional, intellectual and social wellness. It is also beneficial in improving balance and coordination, fine and gross motor skills (Anderson et al, 2019), as well as providing positive sensory stimulation.
So what is therapeutic horseback riding and how does it improve autism associated symptoms? Therapeutic horseback riding (TR) or equine assisted therapy is an activity used with individuals with autism and other special needs. It is used for the purpose of improving physical, emotional, intellectual and social wellness. It is also beneficial in improving balance and coordination, fine and gross motor skills (Anderson et al, 2019), as well as providing positive sensory stimulation. There are many thoughts on Applied Behavioral Analysis (ABA) therapy in autism. These controversial notions concern whether ABA therapy is abusive to children with
There are many thoughts on Applied Behavioral Analysis (ABA) therapy in autism. These controversial notions concern whether ABA therapy is abusive to children with 
